Inconsistent Medicaid Coverage is Associated with Negative Health Events for People with Epilepsy
Abstract
Objective. Examine the association between gaps in Medicaid coverage and negative health events (NHEs) for people with epilepsy (PWE).
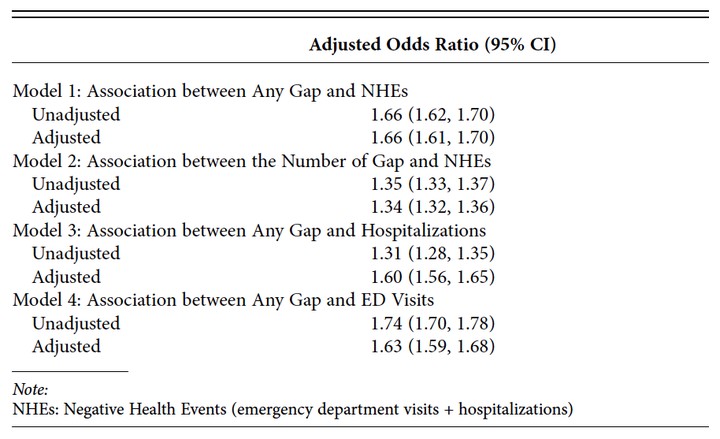
Methods. Using five years of Medicaid claims for PWE, we identified gaps in Medicaid coverage. We used logistic regression to evaluate the association between a gap in coverage and being in the top quartile of NHEs and factors associated with having a gap. These models adjusted for: demographics, residence, medication adherence, disease severity, and comorbidities.
Results. Of 186,616 PWE, 21.7% had a gap in coverage. The odds of being in the top quartile of NHEs per year were 66% higher among those with a gap (OR: 1.66; 95% CI: 1.61, 1.70). Being female, younger, and having psychiatric comorbidities increased the odds of having a gap.
Conclusions. Gaps in Medicaid coverage are associated with being a high utilizer during covered periods. Specific groups could be targeted with interventions to reduce churning.