Abstract
Background: For newly diagnosed people with epilepsy (PWE), proper treatment is important to improve outcomes, yet limited data exist on markers of quality care.
Objective: Examine markers of quality care for newly diagnosed PWE.
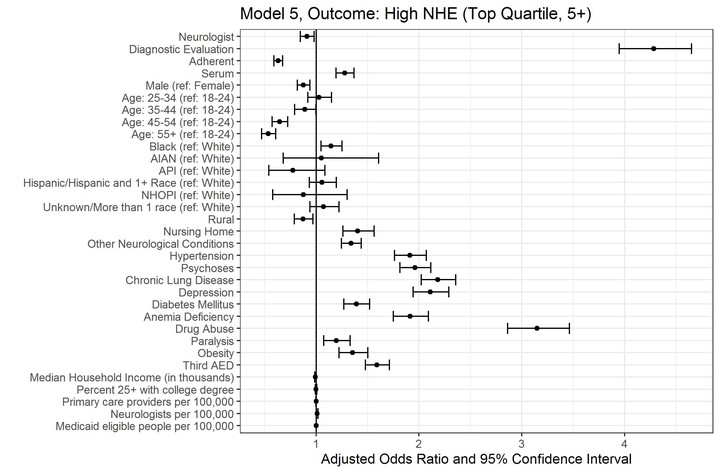
Methods: Using Medicaid claims data (2010-2014) for 15 states we identified adults 18-64 years of age diagnosed with incident epilepsy in 2012 or 2013. We built 5 sequential logistic regression models to evaluate: (1) seeing a neurologist; (2) diagnostic evaluation; (3) antiepileptic medication adherence; (4) serum drug levels checked; and (5) being in the top quartile of number of negative health events (NHEs). We adjusted for demographics, comorbidities, county-level factors, and the outcomes from all prior models.
Results: Of 25,663 PWE, 37.3% saw a neurologist, with decreased odds for those of older age, those residing in counties with low-density of neurologists, and certain race/ethnicities; about 57% of PWE received at least 1 diagnostic test; and nearly 62% of PWE were adherent to their medication. The most common comorbidities were hypertension (37.1%) and psychoses (26.9%). PWE with comorbidities had higher odds of seeing a neurologist and to have NHEs. Substance use disorders were negatively associated with medication adherence and positively associated with high NHEs.
Conclusions: There are notable differences in demographics among people with incident epilepsy who do or do not see a neurologist. Differences in NHEs persist, even after controlling for neurologist care and diagnostic evaluation. Continued attention to these disparities and comorbidities is needed in the evaluation of newly diagnosed PWE.