Racial and Ethnic Differences in Antiseizure Medications Among People With Epilepsy on Medicaid: A Case of Potential Inequities
Abstract
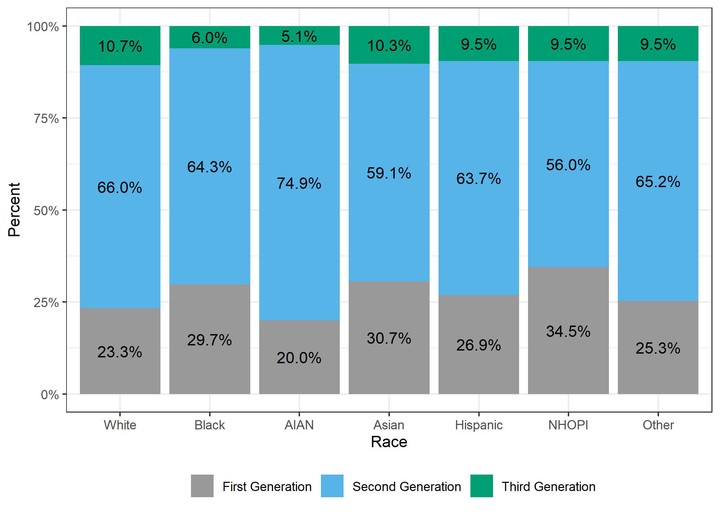
Background and Objectives: Being on a newer, second-, and third-generation antiseizure medication (ASM) may represent an important marker of quality of care for people with epilepsy. We sought to examine whether there were racial/ethnic differences in their use. Methods: Using Medicaid claims data, we identified the type and number of ASMs, as well as the adherence, for people with epilepsy over a 5-year period (2010–2014). We used multilevel logistic regression models to examine the association between newer-generation ASMs and adherence. We then examined whether there were racial/ethnic differences in ASM use in models adjusted for demographics, utilization, year, and comorbidities. Results: Among 78,534 adults with epilepsy, 17,729 were Black, and 9,376 were Hispanic. Overall, 25.6% were on older ASMs, and being solely on second-generation ASMs during the study period was associated with better adherence (adjusted odds ratio: 1.17, 95% confidence interval [CI]: 1.11–1.23). Those who saw a neurologist (3.26, 95% CI: 3.13–3.41) or who were newly diagnosed (1.29, 95% CI: 1.16–1.42) had higher odds of being on newer ASMs. Importantly, Black (0.71, 95% CI: 0.68–0.75), Hispanic (0.93, 95% CI: 0.88–0.99), and Native Hawaiian and Other Pacific Island individuals (0.77, 95% CI: 0.67–0.88) had lower odds of being on newer ASMs when compared with White individuals. Discussion: Generally, racial and ethnic minoritized people with epilepsy have lower odds of being on newer-generation ASMs. Greater adherence by people who were only on newer ASMs, their greater use among people seeing a neurologist, and the opportunity of a new diagnosis point to actionable leverage points for reducing inequities in epilepsy care.